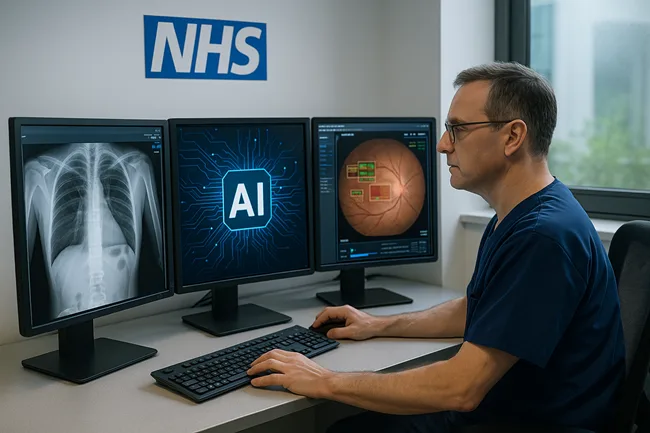
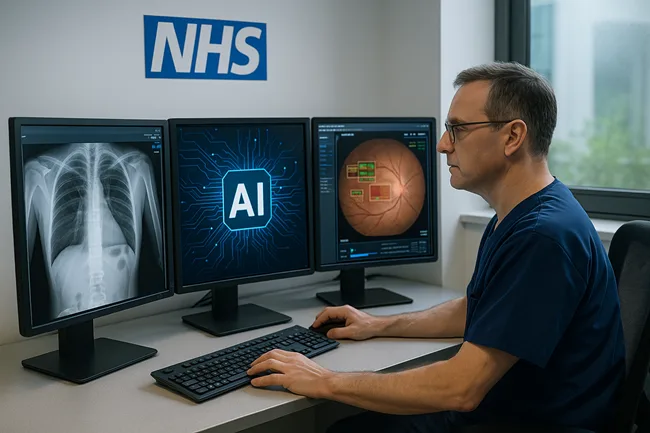
NHS England is accelerating the deployment of artificial intelligence (AI) technologies in both patient triage and diagnostics, as part of its broader Plan for Change and Elective Care Recovery strategy. These efforts aim to modernise healthcare delivery, reduce patient wait times, and improve clinical accuracy across overstretched public hospitals and general practice clinics. Driven by a multi-year policy shift toward digital-first healthcare and supported by targeted funding through the NHS AI Lab, 2025 is emerging as a pivotal year for the integration of AI across frontline services. With dozens of NHS trusts already piloting AI tools for X-ray triage, cancer detection, and automated symptom assessment, the system is beginning to show early signs of transformation.
Why the NHS is using AI for patient triage in 2025
Triage is often the first critical decision point in a patient’s care journey, especially in emergency departments and urgent care clinics. NHS trusts across the country are now adopting AI-based triage platforms to streamline how patients are prioritised. These AI systems—often developed in partnership with UK-based and international medtech vendors—analyse patient symptoms, medical histories, and demographic risk factors to help clinicians determine urgency and route patients accordingly. Unlike manual triage methods that can vary significantly by staff member or time of day, AI systems offer standardised assessments in real time. At trusts like Milton Keynes University Hospital and University Hospitals Birmingham NHS Foundation Trust, AI-powered triage assistants are being trialled to reduce waiting room times and improve decision-making during high-demand periods.
According to NHS England’s Clinical Transformation Directorate, the wider rollout of AI-assisted triage is projected to reduce clinical variation by up to 25% and improve throughput across A&E departments. While clinical oversight remains mandatory, these tools are viewed as force multipliers in an environment constrained by workforce shortages and demand surges.
How AI is reshaping NHS diagnostics across specialties
Beyond triage, NHS England is advancing AI adoption in diagnostic imaging and pathology, where backlogs are particularly acute. AI algorithms are being used to interpret chest X-rays, detect early signs of cancer, and flag high-risk patients in national screening programmes. At Moorfields Eye Hospital NHS Foundation Trust, in collaboration with DeepMind (now part of Google Health), AI models are being applied to optical coherence tomography (OCT) scans to identify eye diseases like diabetic retinopathy and macular degeneration with high accuracy. Meanwhile, at Royal Surrey NHS Foundation Trust, breast cancer screening workflows are being supported by AI systems that help radiologists identify suspicious lesions more consistently across double-read mammograms.
NHS England reported in its 2025 digital progress update that over 60 NHS sites are currently using AI in radiology workflows. These tools are designed not to replace radiologists but to pre-sort and prioritise high-risk images, reduce false negatives, and optimise workload distribution in departments still recovering from COVID-era diagnostic delays. In one example, the deployment of an AI tool for chest X-ray triage at an East Midlands trust reduced average report turnaround time from 12 days to under 48 hours—resulting in earlier cancer referrals and treatment planning.
What funding is enabling NHS AI integration?
The primary financial driver behind these deployments is the NHS AI in Health and Care Award—a £140 million innovation pipeline launched by the Department of Health and Social Care and NHSX. The award is structured in four phases, funding products at different stages of readiness, from early feasibility to large-scale deployment and evaluation. Several AI developers, including UK startups like Kheiron Medical, Brainomix, and Ultromics, have received grants to scale their tools in live NHS environments. In Phase 4 alone, over £55 million was allocated to mature products to support real-world evaluation and procurement readiness.
Institutional observers see the Award not only as a tech adoption mechanism but also as a quality filter. AI firms validated through NHS trials often gain greater investor traction in follow-on rounds or secure export deals based on NHS adoption credibility.
Which NHS trusts are leading in AI pilot programs?
As of June 2025, over 25 NHS trusts are actively piloting or scaling AI systems across clinical domains. Cambridge University Hospitals NHS Foundation Trust is piloting AI-driven lung cancer detection on low-dose CT scans. Guy’s and St Thomas’ NHS Foundation Trust is using radiology AI to prioritise emergency imaging reports. University Hospitals Birmingham has integrated AI for A&E symptom triage and early diagnostics. South Tees Hospitals NHS Foundation Trust is trialling AI-powered dermatology classification for digital referrals.
Many of these pilots are being overseen by NHS Transformation Directorate teams with support from the Academic Health Science Networks (AHSNs), ensuring that evaluation criteria, patient safety standards, and user training are consistent. Dr. Vin Diwakar, Medical Director for Transformation at NHS England, noted in a recent update that “AI is helping the NHS focus clinician time where it matters most—on complex decision-making, not administration or queuing backlogs.”
How are safety, transparency, and bias being managed?
As AI systems become more embedded in clinical practice, NHS Digital and the Medicines and Healthcare products Regulatory Agency (MHRA) have strengthened regulatory frameworks to ensure transparency, explainability, and safety. Under the post-Brexit UKCA (UK Conformity Assessed) regime, AI tools classified as medical devices must undergo rigorous clinical validation, cybersecurity assessments, and data bias audits. NHS England has also instituted independent evaluation boards to assess AI claims before national rollout can occur.
Crucially, tools that demonstrate racial or gender bias—or fail to perform across varied population groups—are not eligible for scale deployment. The NHS AI Ethics Lab, set up in 2024, is leading efforts to ensure that all NHS-deployed AI adheres to principles of fairness and accountability.
What is the expert and institutional sentiment?
Health policy experts from institutions such as the King’s Fund and the Nuffield Trust have broadly supported the NHS’s move toward AI adoption, describing digital augmentation as a practical response to the challenges of rising patient demand and persistent workforce pressures. At the same time, analysts and clinicians have cautioned against over-reliance on automation and have emphasised the importance of long-term investment in staff training, system integration, and governance frameworks. Anecdotal feedback from NHS clinicians involved in early AI deployments has reflected cautious optimism, with many reporting improvements in clinical efficiency and workflow support. However, concerns about tool reliability, accountability, and seamless integration with legacy systems continue to surface, particularly in under-resourced or smaller NHS trusts.
Investor sentiment has also been buoyed by NHS adoption. UK-based medtech firms backed by AI in Health and Care Award funding have reported increased interest from institutional investors and strategic buyers—particularly those looking to scale AI platforms into Europe or the Middle East.
What is the future of AI in the NHS beyond 2025?
NHS England’s long-term strategy envisions AI as a horizontal enabler across most care pathways. Beyond diagnostics and triage, areas under active exploration include AI-generated discharge summaries and documentation, predictive analytics for hospital bed management, intelligent scheduling tools for elective surgery optimisation, AI chatbots and symptom checkers integrated into the NHS App, and population health modelling for early outbreak detection.
The NHS App, with over 20 million users, is expected to become a central interface for AI-powered tools in the community setting. Upcoming pilots will explore embedding virtual triage bots, real-time pre-assessment screening, and personalised reminders for chronic disease management. As NHS trusts gain experience with clinical-grade AI, and as more tools gain regulatory approval under the UKCA process, the digital shift is expected to move from pilot to platform.
Discover more from Business-News-Today.com
Subscribe to get the latest posts sent to your email.